Foretelling the future is often the stuff of science fiction but for a team of scientists at the Novartis Institutes for BioMedical Research (NIBR), it’s their end goal. Led by Juliet Williams, Director of Oncology Pharmacology, and Bill Sellers, Global Head of Oncology, the team has developed a unique system to help predict how cancer drugs might fare well before they enter clinical testing: Are they effective? What types of cancers do they target? Which patients are most likely to benefit from them?
To answer these questions, the team took tumor fragments isolated directly from cancer patients and grew them in mice. Unlike traditional cell line models, this tissue has never touched plastic culture dishes. When scaled across hundreds of patients with many different types of cancer, the approach resembles a kind of clinical trial — but one conducted in mice, not humans. A paper describing this approach appears online in Nature Medicine on October 19.
“This really mirrors a clinical trial,” says Williams. “Typically, you have a person with her own unique tumor and that person gets one dose or one regimen of a drug or combination of drugs. In this case, it’s not a person — it’s a mouse bearing a human tumor.”
A key strength of this approach flows from the fact that patients’ cancer cells never touch a laboratory dish. The mere act of growing tumors on plastic can change their inherent properties, causing some cells to die off and others to rapidly proliferate — leaving behind a caricature of the original tumor, not a genuine replica.
In contrast, implanting tumors in mice, by creating what is known as patient-derived tumor xenograft (PDX) mice, can more faithfully capture the complex biology of human cancers. Since not all tumors are equivalent — the broken genes that drive one person’s lung cancer are different from those that drive another’s, for example — the method can also be appropriately scaled to represent the genetic diversity that exists among various cancer types.
“PDX mice are so powerful because they can capture the genetic heterogeneity that exists within one patient’s tumor and across many patients’ tumors,” says Hui Gao, first author of the study and a Senior Investigator in Oncology at NIBR. “That combination holds enormous promise for our ability to predict up front which drugs might help which patients.”
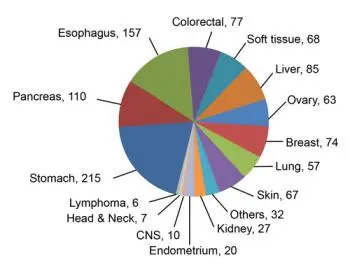
By harnessing this powerful method, Williams, Gao and their colleagues created a compendium of roughly 900 different PDX models spanning major solid tumor types in adult patients. To facilitate the use of these models for testing large numbers of compounds, they first wanted to know if a one mouse, one tumor, one treatment approach would be feasible. It turns out this 1x1x1 method yields highly reproducible results, making it a practical approach to follow as they scaled up their tests. Another key advantage of this “PDX mouse clinical trial” is that tumors from one patient can be implanted in multiple mice, allowing subsequent tests against various different cancer drugs.
To determine how this mouse clinical trial stacks up against those done in humans, Williams, Gao, and their colleagues assembled a pharmaceutical toolkit comprised of more than 60 different anti-cancer treatment regimens. These included both single agents as well as drug combinations. They also included candidate drugs now undergoing clinical testing, compounds still undergoing pharmaceutical development, and therapies now considered a standard of clinical care. They tested this pharmacopeia against more than 250 PDX mouse models, using the 1x1x1 approach.
Remarkably, the mouse clinical trial confirmed several things that were already known from previous human clinical trials. For example, among mice carrying melanoma tumors, roughly 30% of those with mutations in a key gene, called B-RAF, failed to respond to drugs targeting those gene mutations. This is similar to what has been observed in human studies.
The mouse trial also revealed its capacity for uncovering novel insights, such as potential new combinations of cancer drugs — like the addition of a drug known as a CDK4/6 inhibitor to the B-RAF inhibitor treatment often given to melanoma patients. This combination had not been previously thought to be effective, but the new study suggests it could be.
“We’re encouraged by the data,” says Lilli Petruzzelli, who heads the global team responsible for designing human oncology trials at NIBR. “These early results have helped us design more focused combination clinical studies that have the potential to bring benefit to patients.”



