When Collette Thain took a trip to Ireland from her home in Edinburgh, Scotland to watch a rugby tournament in 1994, she never expected to end up in the hospital. She became ill suddenly and was admitted with mysterious signs of liver failure.
Months later, Collette was diagnosed with a rare liver disease called primary biliary cirrhosis (PBC1). Her doctor said there were no approved treatments available, and she had about five years to live. Collette, then 37 and a mother of young children, was flabbergasted. “I asked the doctor, ‘Do you at least have a leaflet?’” she says. “But he wasn’t aware of any resources for me.”
A few years later, Collette began taking ursodeoxycholic acid after it was approved for the treatment of PBC. She responded well and is still taking it today. But about 40% of PBC patients do not respond. For them, the disease progresses and suffering continues. Ultimately, the only option is liver transplantation, which isn’t always possible due to the shortage of organ donors. In addition, it’s a serious procedure with long-term implications.
Novartis researchers are working on an alternative for these patients. Testing of a new compound has begun in patients with PBC who do not respond to the standard therapy. The compound might have a wider reach, however, because lab studies suggest that it combats liver scarring, which occurs in all common forms of liver disease.
“Unless the disease is caused by a hepatitis B or C virus, we are generally relying on archaic treatments for it,” says Nikolai Naoumov, a seasoned hepatologist and Therapeutic Area Head of the liver program at Novartis Pharmaceuticals.
Take non-alcoholic steatohepatitis (NASH), or fatty liver disease, which is increasingly common due to the worldwide obesity epidemic. As fat builds up in the liver, the organ becomes inflamed and damaged. There are no approved therapies for NASH. It is on the rise in Asia, the Middle East and Latin America and has become the primary cause of chronic liver disease in North America and Europe.2 In the United States, it is now the second leading cause of liver transplantation.3
“There is a tidal wave of metabolic liver disease sneaking up on us,” says Michael Badman, Translational Medicine Expert at the Novartis Institutes for BioMedical Research. “We want to provide patients with treatment options beyond liver transplants.”
Scarring: the common path of liver disease progression
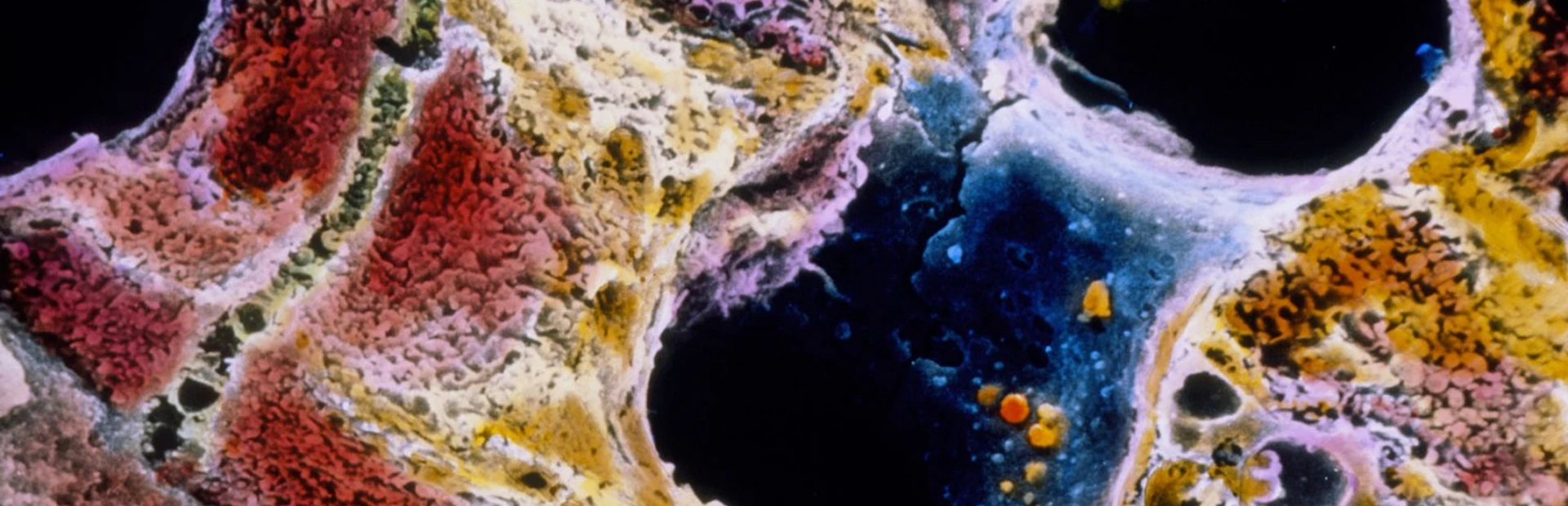
Most forms of liver disease follow the same trajectory. It starts with a trigger, such as a virus or alcohol abuse. In PBC, the trigger is an autoimmune reaction that mistakenly destroys bile ducts in the liver, and in NASH, it is a buildup of fat in the liver. The trigger initiates a vicious cycle of chronic inflammation and liver scarring called fibrosis. If untreated, fibrosis becomes cirrhosis, which can lead to liver failure and, barring a transplant, death.
“Whatever the insult to the liver is, the general pathobiology of liver damage follows the same pathway,” says Naoumov.
For a long time, the idea that a scarred liver could heal was considered a non-starter among liver specialists, but in recent years, there is increasing evidence suggesting that recovery is possible even in late-stage disease. In experiments in mice, the Novartis compound had an anti-scarring effect, suggesting that it might be possible to speed liver healing with medicine.
Scarring in the liver resembles the scarring of the skin. Injuries are repaired with fibrous tissue rather than functional cells. This scar tissue blocks the flow of blood and other biochemicals through the liver, initiating a chain reaction that causes damage.
For instance, the liver produces bile acid to aid digestion. Bile acid dissolves fats in the digestive tract much the way laundry soap washes away stains. But in a scarred liver, bile acid gets stuck and causes more scarring. “Instead of dissolving fats, bile acid trapped in the liver will dissolve things like cell membranes and cause cells to die,” says Bryan Laffitte, Director of Discovery Pharmacology at the Genomics Institute of the Novartis Research Foundation.
The new Novartis compound, which was discovered by Laffitte’s group, is designed to break this cycle. It harnesses the body’s built-in mechanisms for coping with excess bile acid, which builds up in the liver in both PBC and NASH. These mechanisms are governed by a receptor in liver and intestine cells called FXR that detects bile acid and launches protective measures.
“The body turns these processes on naturally, but we’re trying to turn them on more,” says Laffitte.
One way to mimic the natural trigger that flips on the FXR master switch is to create a compound that is derived from a bile acid. But bile acids can also cause unwanted side effects, such as severe itching. The Novartis compound is not derived from a bile acid and is designed to minimize the potential for itch.
Itch is of particular concern for PBC patients. As a symptom of PBC, some experience a maddening itch all over the body, “like an army of ants under the skin,” says Collette, who directs the PBC Foundation patient advocacy group and experiences PBC-related itch on occasion.
Clinical testing begins
Novartis plans to test its new experimental compound in diseases in which bile acid accumulation causes fibrosis and disease progression, such as PBC and NASH. For instance, a clinical trial has begun and will recruit up to 95 PBC patients who have not responded to standard therapy.
This trial follows the Novartis strategy of focusing first on a small and specific group of patients who are likely to benefit and are also in need of therapeutic options, says Badman, who is designing the trials to test the new Novartis compound. The knowledge gained from this initial trial can be put to use in future trials of more complex diseases, like NASH, which progresses in less predictable ways.
Collette still suffers from intense fatigue from PBC, and she still lives day-to-day, despite ongoing treatment. “For so many years there has been little progress for PBC,” she says. “This new compound gives us hope.”